Imaging Through Scattering
Locating and classifying fluorescent tags behind turbid layers using time-resolved inversion
Guy Satat, Barmak Hehsmat, Christopher Barsi, Dav Raviv, Ou Chen, Moungi Bawendi, and Ramesh Raskar
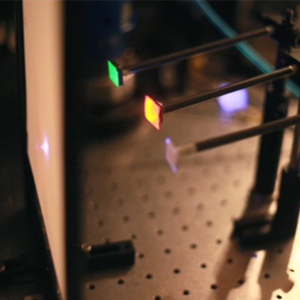 We demonstrate a new method to detect and distinguish among different types of fluorescent materials. The suggested technique, with many biomedical applications, has provided a dramatically larger depth range compared to previous methods; thus it enables medical diagnosis of body tissues without removing the tissue from the body, which is the current medical standard. This method uses fluorescent probes, which are commonly used in medical diagnosis since they can be engineered to attach or change their emission parameters when interacting with specific types of tissues. One of these parameters is the fluorescence lifetime - the average time the fluorescence emission lasts. The new method can distinguish between different fluorescence lifetimes, which allows diagnosis of deep tissues.
We demonstrate a new method to detect and distinguish among different types of fluorescent materials. The suggested technique, with many biomedical applications, has provided a dramatically larger depth range compared to previous methods; thus it enables medical diagnosis of body tissues without removing the tissue from the body, which is the current medical standard. This method uses fluorescent probes, which are commonly used in medical diagnosis since they can be engineered to attach or change their emission parameters when interacting with specific types of tissues. One of these parameters is the fluorescence lifetime - the average time the fluorescence emission lasts. The new method can distinguish between different fluorescence lifetimes, which allows diagnosis of deep tissues.
Locating fluorescence probes in the body using this method can, for example, indicate the location of a tumor in deep tissue, and classify it as malignant or benign according to the fluorescence lifetime, thus eliminating the need for X-ray or biopsy. The method is not limited to biomedical applications and can also be used in industrial and general remote sensing applications, such as inspection, identification and flowmetry.
Paper in Nature Communications
"Locating and classifying fluorescent tags behind turbid layers using time-resolved inversion"Nat. Commun. 6:6796 doi: 10.1038/ncomms7796 (2015),
Guy Satat, Barmak Heshmat, Christopher Barsi, Dan Raviv, Ou Chen, Moungi G. Bawendi, and Ramesh Raskar
http://www.nature.com/ncomms/2015/150413/ncomms7796/full/ncomms7796.html
Abstract
The use of fluorescent probes and the recovery of their lifetimes allow for significant advances in many imaging systems, in particular medical imaging systems. Here, we propose and experimentally demonstrate reconstructing the locations and lifetimes of fluorescent markers hidden behind a turbid layer. This opens the door to various applications for non-invasive diagnosis, analysis, flowmetry and inspection. The method is based on a time-resolved measurement which captures information on both fluorescence lifetime and spatial position of the probes. To reconstruct the scene the method relies on a sparse optimization framework to invert time-resolved measurements.This wide-angle technique does not rely on coherence, and does not require the probes to be directly in line of sight of the camera, making it potentially suitable for long-range imaging.
Applications
The main application of our method is for in-vivo medical diagnosis. Today fluorescent markers are used as contrast agents in standard CT scans and biopsies. Our suggested method enables "in-vivo biopsy".For example, by locating the fluorescent marker we know where a tumor might be, and fluorescence lifetime will classify the tumor as malignant or benign.
Materials and publications:
- Nature Communications paper.
- Nature Communications paper supplement.
- Review paper in SPIE.
- CLEO abstract.
- Masters Thesis.
Paper citations:
- G. Satat, B. Heshmat, C. Barsi, D. Raviv, O. Chen, M.G. Bawendi and R. Raskar, “Locating and Classifying Fluorescent Tags Behind Turbid Layers Non-Invasively Using Sparsity-Based Time-Resolved Inversion,” Nature Communications, vol. 6, 6796 (2015).
- G. Satat, B. Heshmat, N. Naik, A. R. Sanchez and R. Raskar, "Advances in ultrafast optics and imaging applications," in SPIE Commercial Sensing 2016 (oral, invited).
- G. Satat, C. Barsi, B. Heshmat, D. Raviv, and R. Raskar, "Locating Fluorescence Lifetimes Behind Turbid Layers Non-Invasively Using Sparse, Time-Resolved Inversion," in OSA CLEO 2014 (poster).
Frequently Asked Questions:
What are we trying to do?
Allow non-invasive in-vivo detection and classification of tumors.
How is diagnosis of tumors performed today?
Doctors will use medical imaging techniques (like CT) to detect possible locations of tumors. Classification of a tumor as malignant or benign usually requires extracting a piece of that tissue for biopsy and analyzing it under a microscope. A widely used method for such analysis is FLIM (florescence lifetime imaging), where the fluorescence lifetime provides information on the surrounding tissue. However, FLIM requires extraction of the tissue from the body.
What's new in our approach?
Our method allows to measure the florescence lifetime while the fluorophore is embedded within the tissue. Thus, there is no need for invasive measures such as tissue extraction. To accomplish this, our method is based on a time-resolved measurement and signal processing algorithms that localize and classify the fluorescent tags behind scattering layers.
What's the potential impact?
The long term goal can potentially shorten diagnosis cycles and reduce the number of invasive procedures, thus improving the overall health diagnosis process and reduce costs within the healthcare system.
What are fluorescent markers?
Fluorescent markers are widely used as contrast agents in CT and MRI scans. They are also an important tool when performing biopsies.
What is fluorescence lifetime?
When the fluorophore is excited, the fluorescence isn’t emitted immediately. The time that passes before the emission is known as the fluorescence lifetime (which is an average, since the process is random). This time can be a function of the environment, and so it is an important tool that can assist in classifying the fluorophore environment.
What is a streak camera?
A streak camera is a device that captures time information along a line in space (each column corresponds to a different location along the line, and each row corresponds to a different time). When a light pulse enters the instrument through a narrow slit along one direction, it is deflected in the perpendicular direction, so that photons that arrive first hit the detector at a different position compared to photons that arrive later. The resulting image forms a “streak” of light. Streak tubes are often used in chemistry or biology to observe millimeter-sized objects.
What's the depth limitation of the system?
In this project we demonstrated the concept on a 0.7mm thick opaque glass. However, due to the great signal-to-noise properties of our algorithm, it can work in deep tissues as well. The limitation on depth is due to time blur from the scattering, which should be on shorter time scales than the fluorescence lifetime.
Why patches?
Fluorescence markers tend to generate sparse images. We use a sparsity prior as part of the reconstruction algorithm to make it more robust.